A new study, SYNTAX III REVOLUTION, has found heart teams using computed tomography (CT) angiography to decide between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) to treat patients with three-vessel/left main disease would agree with 92.8% of decisions made by heart teams using conventional angiography. This creates a Cohen’s Kappa of 0.82, which represents almost perfect agreement.
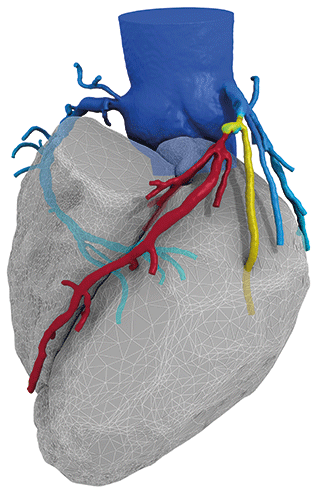
Presenting the results of SYNTAX III REVOLUTION at EuroPCR (22 May—25 May, Paris, France), Patrick Serruys (Imperial College, London, UK), noted that “in the last two decades” CT angiography has been introduced as a non-invasive alternative for coronary anatomy assessment. He added that CT angiography has been shown to be a safe and feasible approach for calculating the anatomical SYNTAX score (used for assessing the extent of coronary artery disease and choosing the most appropriate revascularisation strategy).
The aim of the present study was to evaluate how CT angiography compares with conventional angiography in assessing patients with three vessel or left main disease. The primary endpoint was the first decision making and treatment strategy based on anatomic SYNTAX score and the SYNTAX II score, which combines the anatomical SYNTAX score with a patient’s clinical characteristics.
In the study, six heart teams—each comprising of interventional cardiologists, radiologists, and cardiothoracic surgeons—were randomised into one of two groups: heart team A and heart team B (with three teams in each group). Heart team A had to decide treatment based on conventional angiography and heart team B had to decide treatment based on CT angiography (Revolution, GE Healthcare) alone. Heart team B also had to evaluate whether the use of fractional flow reserve (FFR) CT analysis (FFRCT, HeartFlow) would change their initial treatment decision. FFRCT, via a computer algorithm, using information from a CT angiogram to calculate FFR values.
Using data from 223 patients of the original SYNTAX study, overall, the heart team group agreed upon the treatment strategy (CABG or equipoise between PCI and CABG) in 92.8% of cases. This led to a Cohen’s Kapa of 0.82, which Serruys claimed represented “an almost perfect agreement” between the two groups.
Additionally, the heart team groups agreed upon the coronary segments to be revascularised in 81.1% of the cases. For heart team B, according to Serruys, the use of FFRCT changed the treatment decision in 7% of patients. In 13 patients, the treatment changed from a surgical approach to a percutaneous one.
“In patients with left main or three vessel coronary artery disease, a heart team treatment decision-making based on coronary CT angiography showed an almost perfect agreement with the decision derived from conventional angiography suggesting the potential feasibility of a treatment decision-making and planning and solely on this non-invasive imaging modality,” Serruys concluded.
He added that a first-in-human study would further explore the use of CT angiography to make treatment decisions.










