Among patients with heart failure and reduced ejection fraction (HFrEF), those taking a once daily “polypill” combination of three heart failure medications, had improved heart function and symptoms, better quality of life, fewer hospitalisations and greater medication adherence in comparison to those who took the same medications as separate pills for six months.
“In recent decades, there have been important, effective treatment advances for patients with heart failure, however, use of these treatments remains disappointingly low, with only 15% of patients receiving all guideline-recommended therapies at any dose for heart failure after hospitalisation,” said study author Ambarish Pandey (UT Southwestern Medical Center, Dallas, USA) who presented the findings at the American Heart Association (AHA) 2025 scientific sessions (7–10 November, New Orleans, USA). “In our study, we focused on socially disadvantaged populations to demonstrate the positive impact of an easier-to-follow medication regimen of only one pill versus three pills daily, and we found significant improvements even after six months. Our findings provide the first evidence that a polypill approach could be effective for our patients with heart failure.”
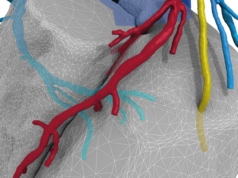
The trial included 212 adults with HFrEF who were not receiving guideline-recommended treatment. Participants were randomly assigned to one of two groups: 108 participants were prescribed the polypill regimen, which included metoprolol succinate (a beta-blocker), spironolactone (a mineralocorticoid receptor antagonist) and empagliflozin (a SGLT2 inhibitor). The second group of 104 adults were assigned to enhanced standard care, taking guideline-recommended medications as individual pills. Everyone also took an angiotensin receptor-neprilysin inhibitor (ARNI), sacubitril-valsartan, which is dosed twice-daily and not well suited for a once-daily polypill.
After six months, the study found neasures of left ventricular ejection fraction (LVEF) improved among all participants, with a 3% higher absolute LVEF among the polypill group versus the enhanced standard care group. The polypill reduced heart failure-related hospitalisations and emergency room visits by 60%—meaning patients in the polypill group were less than half as likely to need emergency care. Patients in the polypill group reported higher quality of life scores than those in the enhanced standard care group (72 points vs. 63 points, on a 100-point scale). This approximate nine-point improvement means patients experienced less fatigue, fewer symptoms, and better overall well-being.
Blood tests confirmed that 79% of polypill patients had detectable levels of the tested medications (metoprolol and/or spironolactone), compared to only 54% in the enhanced standard care group, with more than four-fold greater odds of taking all tested medications with the polypill.
The study group plans more research on how best to address heart failure in specific groups. “Moving forward, we are planning additional studies to evaluate broader implementation of the polypill approach in heart failure,” Pandey said.