A pilot study comparing a strategy of left ventricular unloading with the Impella CP device (Abiomed) and delayed reperfusion (up to 30 minutes after left ventricular unloading) with a strategy of left ventricular unloading and immediate reperfusion for the management of ST-segment elevation myocardial infarction (STEMI) indicates that delaying reperfusion does not increase infarct size or increase the risk of major adverse cardiovascular or cerebrovascular events (MACCE). These findings suggest a larger trial of left ventricular unloading and delayed reperfusion would be safe to perform.
Writing in Circulation, Navin K Kapur (The CardioVascular Center and The Molecular Cardiology Research Institute, Tufts Medical Center, Boston, USA) and others report that unloading the left ventricle prior to coronary reperfusion reduces ischaemia-reperfusion injury and myocardial infarct size in acute myocardial infarction (vs. reperfusion alone). “More recently, preclinical testing identified that unloading the left ventricle and delaying reperfusion by 30 minutes activates a cardioprotective signalling programme that reduces myocardial damage after reperfusion and promotes myocardial recovery 30 days after acute myocardial infarction,” they add.
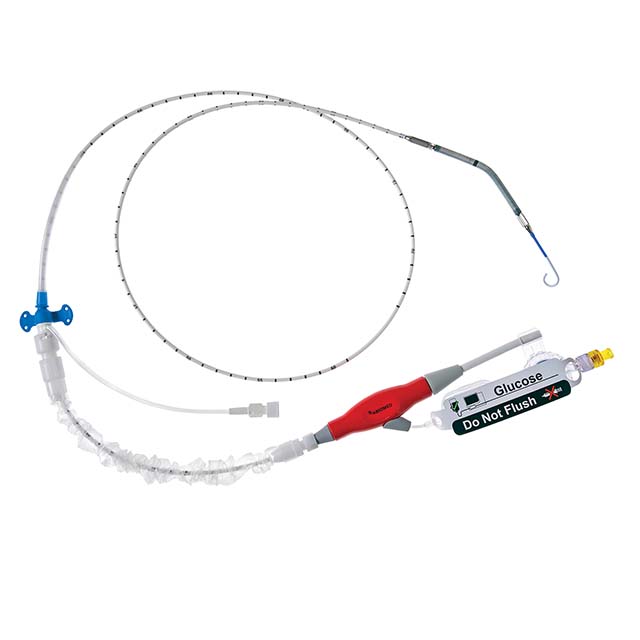
However, the authors comment that “any delay to reperfusion is not recommended” in the context of STEMI and that Impella CP (a device for left ventricular unloading) is not indicated for STEMI patients who do not have cardiogenic shock. Furthermore, for every 30 minute delay to reperfusion, one would expect a significant increase in myocardial damage. Therefore, to “inform the development of an appropriately powered randomised controlled study comparing the efficacy of a left ventricular unloading strategy with the current standard of care for STEMI”, Kapur et al conducted the Door-to-Unload in STEMI pilot trial.
In the study, 50 STEMI patients were randomised to left ventricular unloading with the Impella CP device and immediate reperfusion (25 patients) and left ventricular unloading (again with the Impella CP) and delayed (up to 30 minutes) reperfusion (25). The primary safety outcome was the rate of MACCE at 30 days and the primary efficacy endpoint was to demonstrate no increase in infarct size as percent of total left ventricular mass at 30 days with unloading and delayed reperfusion.
At 30 days, the trial successfully demonstrated no significant differences between groups in either the primary safety endpoint or the primary efficacy endpoint. As to be expected, the time from unloading to the first coronary angiogram was significantly longer in the delayed reperfusion group: 1.7±6.9 minutes vs. 13.8±10.3 minutes for immediate reperfusion (p<0.01). “Left ventricular unloading using the Impella CP device with a 30-minute delay reperfusion is feasible within a relatively short time period,” Kapur et al say. They add that the pilot study “did not identify any prohibitive safety signals that would preclude proceeding to larger pivotal study of left ventricular unloading before reperfusion and further demonstrated that contrary to current belief, a 30 minute delay to reperfusion on the platform of unloading did not increase infarct size”.
“The DTU-STEMI pilot study overcomes a critical barrier to progress in the field of cardioprotection and myocardial recovery by suggesting for the first time that it is possible to delay coronary reperfusion, thereby allowing enough time for left ventricular unloading to precondition the myocardium and reduce ischaemia-reperfusion injury and overall myocardial damage in acute myocardial infarction,” the authors conclude. They report that “with these observations in mind”, “an appropriately powered pivotal trial comparing left ventricular unloading before reperfusion before reperfusion to the current standard of care in anterior STEMI is in development”, noting that the finding that left ventricular unloading and delaying reperfusion is feasible also “potentially opens many new doors for further exploration by suggesting that other adjunct interventions (i.e. pharmacologic) may now be considered during that ‘window period’ where the coronary artery is occluded but the left ventricular is unloaded”.
Kapur told Cardiovascular News: “The DTU-STEMI pilot trial successfully demonstrated that contrary to our current clinical thinking where any 30-minute delay to reperfusion in STEMI should significantly increase infarct size, a 30-minute delay to reperfusion on the platform of left ventricular unloading does not increase infarct size. These observations support moving forward with the DTU-STEMI pivotal trial where we will test whether left ventricular unloading and delayed reperfusion reduces myocardial damage compared to the current standard.”
Coinciding with its publication in Circulation, the DTU-STEMI pilot study was presented (by Kapur) during a late-breaking trial presentation at the 2018 American Heart Association (AHA) scientific sessions (10–12 November, Chicago, USA).