
This advertorial is sponsored by Medtronic
Durability, reliability, accuracy. These are just some of the characteristics that interventionalists look for in a transcatheter aortic valve implantation (TAVI) device to achieve the predictable results that their patients need in the long run. With TAVI procedures now being performed across a younger, lower-risk patient population, reliable haemodynamic performance, predictable rates of permanent pacemaker implant and proven durability come ever more to the fore.
According to Nicolas Dumonteil (Clinique Pasteur, Toulouse, France), the importance of valve durability is one of the components that is now front and centre in the interventionalist’s mind when planning a TAVI procedure. “It has become more and more important since we have had the extension of indications to patients having a longer life expectancy,” Dumonteil tells Cardiovascular News. “Fifteen years ago, we used to treat patients who had maybe three, four, or five years of life expectancy and therefore valve durability was less of a concern. As we are now treating patients who can have ten or more years of life expectancy, and, for the majority, that are still good surgical candidates, it has become a crucial concern at the time of the first valve selection process.”
Perhaps the most important recent development regarding valve durability is the pooled analysis of five-year data from the CoreValve US Pivotal and SURTAVI trials, delivered by Michael J Reardon (Houston Methodist DeBakey Heart and Vascular Center, Houston, USA) at the American College of Cardiology (ACC) Scientific Sessions (2–4 April, Washington, DC, USA). The study evaluated the five-year incidence and predictors of haemodynamic valve deterioration (using standardised definitions) and clinical outcomes among patients who had been randomised to undergo TAVI—using either the CoreValve or Evolut (Medtronic) platforms—or surgical aortic valve replacement (SAVR).
Researchers looked at 1,484 intermediate-risk (792 TAVI, 692 SAVR) and 615 high-risk (336 TAVI, 279 SAVR) patients for structural valve deterioration (SVD), finding that in patients with symptomatic severe aortic stenosis at intermediate or high surgical risk, the five-year rate of SVD was 4.38% in patients undergoing surgery, versus 2.57% in patients undergoing TAVI using the Evolut and CoreValve platforms (p=0.0095).
“Those data are crucial for our community because we started with TAVI thinking that it was a treatment for patients who were inoperable,” says Dumonteil. “Now, for the first time, we have robust, large-scale data to inform our patients that so far, at five years’ follow-up, with such a platform we do not have to express any concerns regarding valve durability as compared to surgical implants. That is crucial, especially at the time of pre-operative discussion with the patients and explanation of the pros and cons of TAVI and SAVR.”
An important concept to consider is the design of the CoreValve and Evolut platforms—both are self-expanding, supra-annular valves—which potentially explains some of the mechanism behind its performance at five years. Dumonteil says that the findings from the pooled analysis gives weight to the hypothesis that the supra-annular positioning of the leaflets in the CoreValve and Evolut platforms, and the design of thoses leaflets contributes to its promising five-year results.
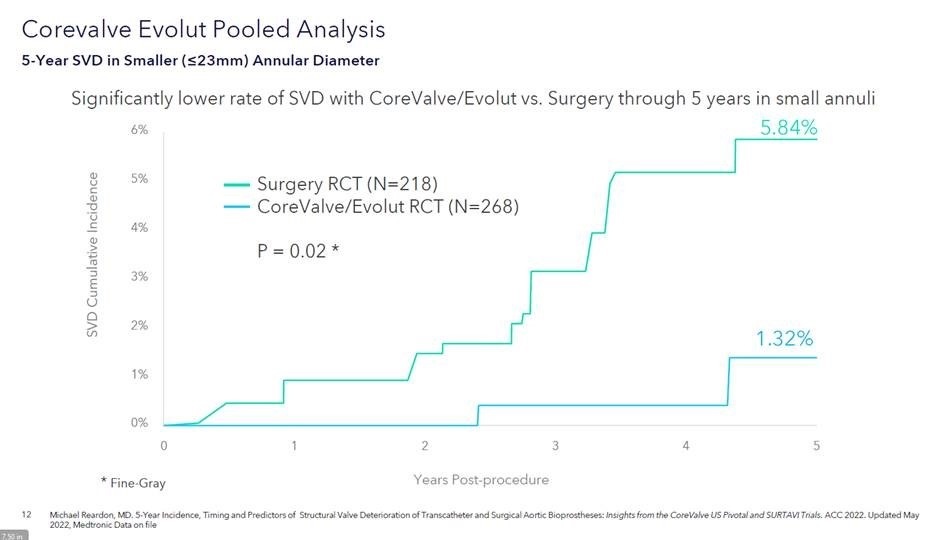
The unique design of the Evolut platform may also confer benefits among patients with small aortic annuli, with the data suggesting that the difference in SVD was observed to be more profound in patients with smaller (≤23mm) annuli (SVD: 5.84% surgery vs. 1.32% TAVI; p=0.049). “The valve has been developed to have a decoupling of the constrained portion of the frame in the small orifice of the aortic annulus. This hypothesis has been mentioned since the early ages of CoreValve implantations, but now we have some data that suggest it could be true,” Dumonteil explains, discussing the theoretical mechanism behind this finding.
This year marks 20 years since the first TAVI procedure was performed by Alain Cribier—in Dumonteil’s native France—and structural heart specialists now benefit from two decades’ worth of experience in planning and executing the procedure. This helps to determine the right strategy, and ensure that the patient is receiving the right valve to match their anatomy. As valve technologies have developed, so have the implant techniques, and an experienced operator will now have knowledge of many technical variations that they can deploy to optimise outcomes in complex cases.
One such new approach is the cusp overlap technique (COT). Cusp overlap is intended to lower the risk of interference with the conduction system, by providing a more accurate assessment of valve depth upon implant, thereby lessening the risk that the TAVI patient may need a pacemaker implantation—which has been a common feature of the procedure. “We need to thank those who proposed to shift to this practice,” says Dumonteil. “They [have] helped us understand that in this projection we have a better understanding of the real and natural depth of implantation in the left ventricular outflow tract (LVOT), and therefore we must be more accurate in terms of implant depth or positioning of the valve.”
The merits of the technique, when used in conjunction with the Evolut valve, has been among the key learnings from the Optimize PRO study, which was conducted among 400 patients treated in the USA and Canada. Recent findings from the study have shown that cusp overlap led to more “predictability and control,” according to investigators, resulting in a single-digit pacemaker implantation rate (9.2%), and upon discharge, no cases of moderate or severe paravalvular leak (PVL; 0%). The lowest pacemaker implantation rates were observed when all steps of the cusp overlap technique were followed, investigators found.
 “It was necessary to have this kind of large-scale registry data to validate these theoretical advantages,” says Dumonteil, of the study. “The most interesting outcome coming from that is to validate, in real-world patients, through a multicentre observational study, that if we use this simple, but rigorous, technique to implant the supra-annular Evolut platform, then we can dramatically increase our procedural outcomes, regarding those two potential complications, that are pacemakers and PVL.”
“It was necessary to have this kind of large-scale registry data to validate these theoretical advantages,” says Dumonteil, of the study. “The most interesting outcome coming from that is to validate, in real-world patients, through a multicentre observational study, that if we use this simple, but rigorous, technique to implant the supra-annular Evolut platform, then we can dramatically increase our procedural outcomes, regarding those two potential complications, that are pacemakers and PVL.”
Taking all of these data together, Dumonteil believes that perception of the TAVI procedure is changing within the interventional cardiology community.
“What has changed, and what is still changing, is that now, at the time of a first transcatheter valve implant, related to the life expectancy of a patient with 10 years of life expectancy after aortic valve treatment, then we must take into account some factors related to this,” he says.
“To end with Evolut—the good thing with the recent data we have at five years, and of course we need the 10-year data—we initially implanted those valves thinking about maybe needing after six, seven or eight years to implant a second one. But, the hope we have now, is that these five-year data will be confirmed at 10 years and finally we will have the proof that the first implant we are doing is the only one the patient will have until the end of their life, and this would be the ideal scenario.”










