Patients with heart failure who had an interatrial shunt inserted between the left and right atria did not see any significant benefits overall compared with those who received a placebo procedure after a median of 22 months follow-up, a study presented at the American College of Cardiology’s (ACC) 2024 annual scientific session (6–8 April, Atlanta, USA).
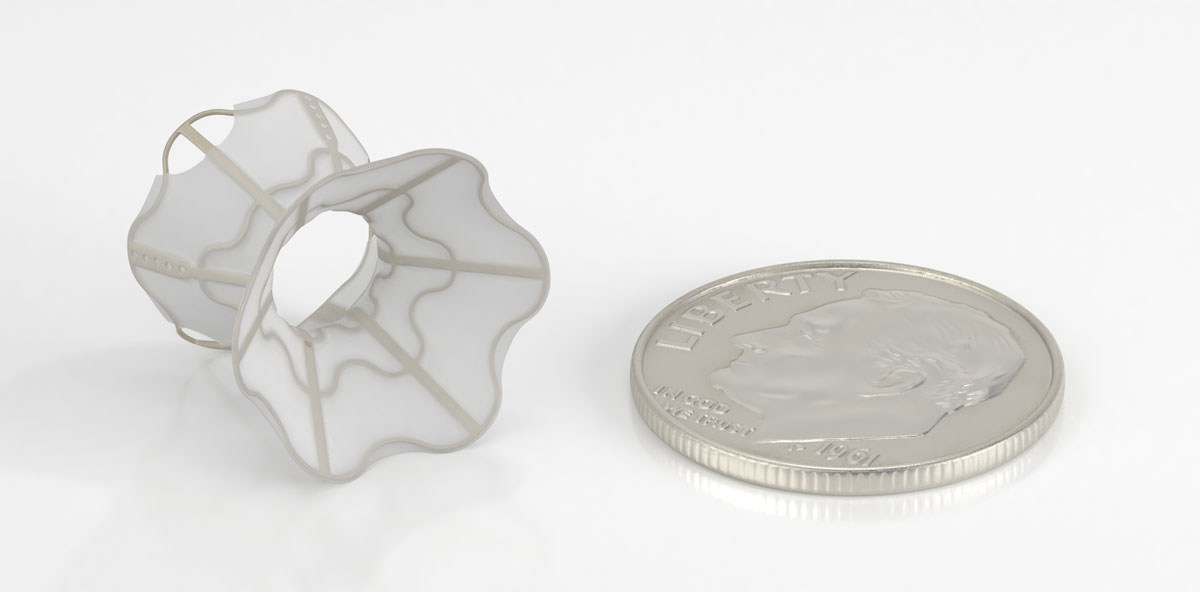
The trial, RELIEVE-HF, is a randomised placebo-procedure controlled trial of interatrial shunting using the Ventura (V-WAVE) device that included patients with both heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF).
Researchers have suggested that though the trial failed to meet its primary endpoint, it does offer some signals that the benefits and risks of interatrial shunts may vary by heart failure type.
“When you examine the outcomes in patients with heart failure across a broad range of left ventricular ejection fraction, the Ventura interatrial shunt was extremely safe but did not improve outcomes compared with no treatment. However, in a prespecified analysis, data suggest that the shunt may be beneficial in patients with HFrEF and worsen outcomes in patients with HFpEF,” said Gregg Stone (Icahn School of Medicine at Mount Sinai, New York, USA), the study’s first author. “We believe further studies are warranted to confirm the benefits we observed in patients with reduced ejection fraction.”
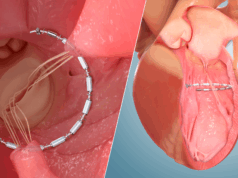
The shunt is designed to create a small amount of blood flow from the left atrium to the right atrium sufficient to lower elevated left atrial pressure while protecting the right heart from failing due to blood volume overload. High left atrial pressure is a primary cause of shortness of breath and hospitalisations related to heart failure.
The trial randomized 508 patients at 94 sites in North America, Europe, Israel, Australia and New Zealand. All participants had symptomatic heart failure despite taking medications at maximally tolerated doses. About 40% of participants had HFrEF and 60% had HFpEF.
Participants were randomly assigned to undergo a procedure to insert the Ventura shunt or a placebo procedure in which a script was followed with all the same protocols to mask patients as to whether the shunt was inserted. Operators were aware of which procedure each patient received but patients, their families and the rest of the medical teams taking care of the patient after the procedure were not. Researchers tracked outcomes in each participant for at least one year and up to two years.
The results showed no significant difference between groups in terms of the trial’s primary endpoint, a hierarchical composite ranking of death from any cause; heart transplant or left ventricular assist device; heart failure hospitalisations; worsening of outpatient heart failure events; and change in quality of life, as measured using the Kansas City Cardiomyopathy Questionnaire (KCCQ). This hierarchical composite approach for assessing efficacy allows diverse types of outcomes to be incorporated in ranked fashion into an overall “win ratio” reflecting the overall outcome of a drug or device.
In a pre-planned analysis focused on heart failure type, patients with HFrEF who received the shunt were found to have improvements across all outcomes assessed (especially fewer hospitalisations for heart failure), while those with HFpEF who received the shunt were found to have increased rates of death and heart failure hospitalisations. This difference could be attributed to the greater compliance or flexibility of the heart muscle with HFrEF, potentially allowing it to more easily accommodate the extra blood flowing into the right atrium, Stone said.
There were no device-related or procedure-related major adverse cardiovascular or neurologic events in either group during the duration of the trial.

Surprisingly, a marked improvement in quality of life as measured with KCCQ was observed across all groups—including those who received a placebo procedure, both with HFrEF and HFpEF—suggesting that the metric may not be a reliable indicator for quality-of-life outcomes in this context, Stone said.
“There was a tremendous placebo effect,” he said. “These observations, especially the fact that quality of life improved in HFpEF patients who were more likely to be hospitalised for heart failure and had reduced survival after shunt treatment, raise questions about the interpretation of this quality-of-life measure in these kinds of trials.”
Although the observed differences in outcomes among people with different types of heart failure may inform future research and development for interatrial devices, the researchers said that the trial was not powered to show differences in the two types of heart failure. As such, these results should be considered exploratory. They also said that the results may not be applicable to other interatrial shunts beyond the Ventura shunt.