Data from 700 patients treated for severe aortic regurgitation (AR) with the Trilogy (Jenavalve) transcatheter aortic valve implantation (TAVI) system in the ALIGN-AR clinical trial have demonstrated the sustained performance of the valve, investigators have said. Added to this, procedural refinements in later stages of the trial point towards improved safety and lower rates of pacemaker implantation associated with the procedure over time.
Raj Makkar (Cedars-Sinai, Los Angeles, USA) presented the latest ALIGN-AR data, the largest cohort available form the trial to date, during a late-breaking trials session at PCR London Valves (16–18 November, London, UK), with the results simultaneously published in The Lancet.
Off-label use of non-AR-specific TAVI valves is associated with high rates of valve embolization and residual paravalvular regurgitation, both of which increase mortality, Makkar said in his presentation of the results. Unlike other available TAVI devices which are primarily engineered for the treatment of aortic stenosis, the Trilogy valve is designed for the treatment of AR with locators that clip onto native leaflets and enable secure anchoring in the absence of calcium.
ALIGN-AR is a multicentre, non-blinded, single-arm study, evaluating the safety and efficacy of the device in patients with symptomatic, severe AR who were considered high risk for surgical aortic valve replacement (SAVR). More than 1,300 patients were screened for inclusion in the trial, which took place at 30 US sites, with 700 patients ultimately enrolled. Of these, 500 patients have reached one-year follow-up and 365 have reached two years. Thirty-day safety outcomes are available in all 700 patients.
Detailing the baseline characteristics of the patient population, Makkar noted that patients had an average age of 79 years, Society of Thoracic Surgeons (STS) Predicted Risk of Mortality (PROM) score of 3.8, 59% were in New York Heart Association (NYHA) class III–IV, and 38.9% had a history of atrial fibrillation (AF).
The Trilogy valve was successfully implanted in 97.7% of cases, with an average procedural time of 67 minutes. General anaesthesia was used in 70% of cases. Technical success was seen in 94.9% of cases, with no procedural deaths among any of the 700 patients. Device success to 30 days was recorded in 96.8% of cases, with 0% prosthesis mismatch.
The trial’s primary safety endpoint, a composite of all-cause mortality, stroke, life-threatening or major bleeding, major vascular complication, acute kidney injury (AKI) ≥2 or dialysis, valve reintervention, new pacemaker implantation or ≥moderate valvular regurgitation occurred in 24% of cases, Makkar reported, primarily driven by high pacemaker rates, but lower than the trial’s overall prespecified performance goal of 40.5%.
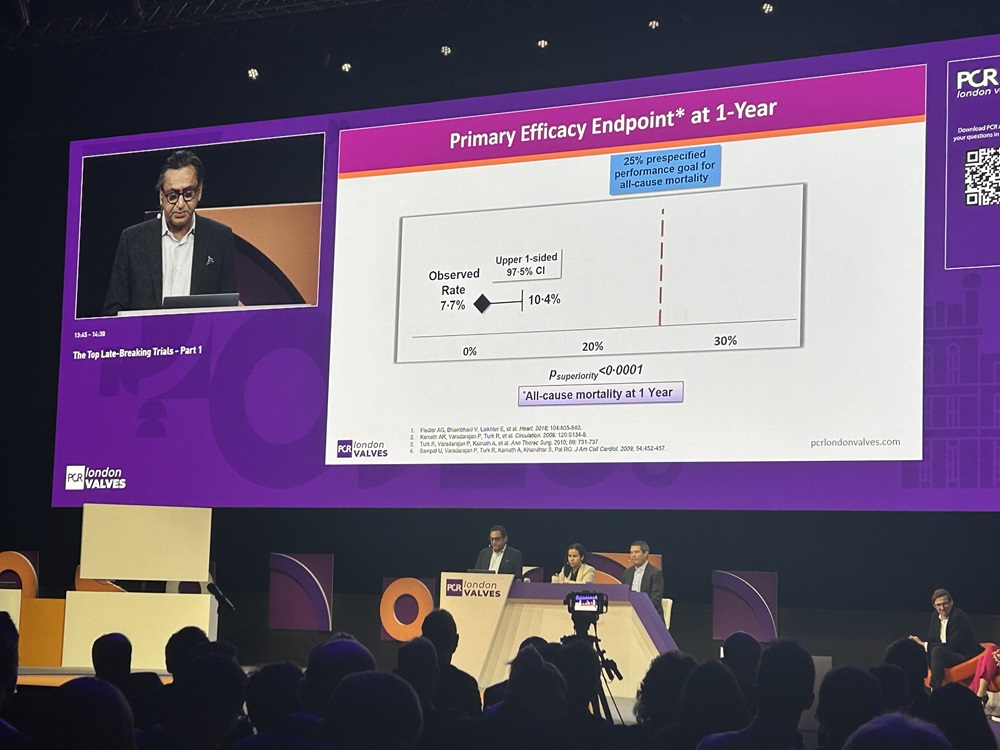
Thirty-day mortality stood at 1.6%, major bleeding 2.7%, and one-year all-cause mortality, the trial’s primary efficacy endpoint, was observed in 7.7% of cases, achieving superiority against the prespecified performance goal of 25%. Mortality increased to 13.3% at two years, Makkar detailed, primarily driven by non-cardiac causes of mortality. He described stroke rates as “acceptable”, with a rate of 0.8% for disabling stroke at 30 days, increasing to 2.2% at two years, and 2.2% for all strokes at 30 days, increasing to 5.6% at two years.
Turning to the haemodynamic performance of the valve, which he described as “excellent”, Makkar reported that the mean aortic valve gradient stood at 3.71mmHg at 30 days and 4.27mmHg at two years, whilst effective orifice areas of 2.99cm2 and 4.27cm2 were recorded at 30 days and two years, respectively.
“This valve was highly effective in treating aortic regurgitation,” Makkar commented, observing that 99% of patients had mild or less residual aortic regurgitation at one and two years. Additionally, Makkar reported that investigators observed “very favourable” left ventricular (LV) remodelling, evidenced by a two-year LV end-diastolic volume of 65mL/m2, LV end-systolic volume of 30.6mLm2, and LV mass index of 107G/m2 at the two-year timepoint.
“We also saw in a tertile analysis, that patients who had the most LV remodelling, patients who had decreased their LV and systolic volume index by most actually had the best clinical outcomes and lowest incidence of death and heart failure hospitalisations,” he detailed.
NYHA functional class improved significantly from baseline, with 92% of patients in either NYHA class I or II at two years, alongside an increase in Kansas City Cardiomyopathy Questionnaire (KCCQ) score of almost 20 points, which was sustained out to this timepoint. Rates of bioprosthetic valve dysfunction were low, Makkar noted, with an aortic valve reintervention rate of 0.8%.
Investigators also sought to analyse any potential impact that increased experience with the device may have on safety outcomes, and performed an analysis of 30-day safety outcomes based upon tertile of enrolment. “What you can see is that the primary composite endpoint decreased from 28.5% to 17.5%, and this was driven by a decrease in new pacemakers, any bleeding complication, as well as any major vascular complications,” Makkar commented.
In their Lancet paper, Makkar and colleagues describe the high rate of new pacemaker implantation as “an area of ongoing concern”, stating that the observed frequency of new pacemaker implantation “remains higher than desired, with approximately one in five patients requiring a new pacemaker at 30 days”.
“The association between larger valve size and greater need for pacemaker might reflect greater circumferential contact and radial force in compliant, non-calcified annuli—increasing mechanical stress near the membranous septum,” they write in their summary of the findings. Similar to a previously reported series on use of the Trilogy valve, pre-existing right bundle branch block (RBBB) was a significant predictor of pacemaker implantation in the study, they state.
Asked to comment on this pacemaker rates in discussion that followed the presentation, Makkar noted that changes in approach to oversizing of the valve had hope of a solution to mitigate this issue.
“We know that aortic regurgitation is a different disease compared to aortic stenosis. Even after surgery, patients who have aortic regurgitation actually have higher pacemaker rates, more like 10–11% rather than 5–6%,” he commented. “One of the things that changed is that we became a little bit conservative in terms of oversizing. When you have valves that could be eligible for both a medium-sized valve or a large-sized valve, I think the trend over the last year or so has been to go ahead in the areas of overlap to use a smaller valve.”