Low-dose intracoronary fibrinolysis infusion during primary percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI) has been shown not to be effective in reducing major adverse cardiovascular events (MACE).
This was the headline finding from the STRIVE multicentre, randomised, double-blind, placebo-controlled trial, in which it was found that low-dose administration of the recombinant tissue plasminogen activator (tPA) alteplase in patients with large-territory STEMI and high thrombus burden undergoing primary PCI did not improve outcomes.
Shamir Mehta (McMaster University and Hamilton Health Sciences, Hamilton, Canada) presented the findings during a late-breaking presentation at the 2025 Transcatheter Therapeutics (TCT) conference (25–28 October, San Francisco, USA), and the data were simultaneously published in the Journal of the American College of Cardiology.
Approximately one-half of patients with apparently successful primary PCI for STEMI have distal embolisation of thrombus causing coronary microvascular obstruction and reduced myocardial tissue perfusion, Mehta detailed. This leads to larger infarct size and higher rates of heart failure, cardiogenic shock and mortality.
The STRIVE trial evaluated a strategy to prevent and treat microvascular obstruction and reduce major cardiovascular events by delivering alteplase, a fibrin-specific thrombolytic, directly into the culprit coronary artery.
Patients who presented with STEMI within six hours of symptom onset and were referred for primary PCI were eligible for the study. All patients were required to have evidence of large territory STEMI on electrocardiogram (ECG) and evidence of large thrombus burden on coronary angiography.
A total of 210 patients were randomised to receive the study drug or placebo (68 received alteplase 10mg, 69 received alteplase 20mg and 70 were given placebo). After antegrade flow was established, a delivery catheter was inserted into the infarct-related artery distal to the culprit lesion and the study drug was infused over three minutes. Primary PCI was performed per standard practice.
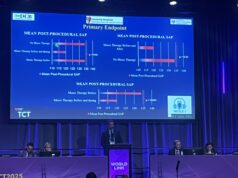
The primary outcome was the composite of MACE at 30 days, Thrombolysis in Myocardial Infarction (TIMI) risk score myocardial blush grade 0/1, distal embolisation or failure to achieve 50% ST segment resolution at 30 minutes post-PCI.
MACE included the first occurrence of cardiovascular death, re-MI, cardiogenic shock and new-onset heart failure at 30 days. The primary safety outcomes were major bleeding or the composite of major bleeding or clinically relevant bleeding at 30 days.
The primary outcome occurred in 73 patients (53.3%) in the alteplase groups versus 37 (52.9%) in the placebo group. Results were consistent across all components of the primary outcome and for each dose group versus placebo. Major or clinically significant bleeding occurred in one patient in the trial (in the alteplase 20mg group). During study drug administration, there were more episodes of ventricular fibrillation in the alteplase groups compared to the placebo group (10.2% vs 1.4%).
“Microvascular obstruction after primary PCI remains the single most important unresolved issue limiting the efficacy of primary PCI in STEMI patients,” said Mehta. “STRIVE does not support the routine administration of alteplase and it joins the growing list of previously promising therapies that have not succeeded in improving this important issue.”