Data from three randomised trials and a meta-analysis presented at the European Society of Cardiology (ESC) congress (25–28 August, Amsterdam, The Netherlands) offer new insights into the use of intravascular imaging—either optical coherence tomography (OCT) or intravascular ultrasound (IVUS)—to optimise outcomes during PCI.
Attendees to Sunday morning’s main arena session heard evidence from the ILUMIEN IV trial, looking at OCT-guided PCI in high-risk patients; the OCTOBER trial, which assessed OCT-guidance in bifurcation lesions; and OCTIVUS, a comparison of OCT and IVUS in a broad population of patients. The session finished with the presentation of a “real-time” updated network meta-analysis, integrating data from both the ILUMIEN IV and OCTOBER trials.
Presenters and panellists broadly agreed that the new data, taken in totality, make a strong case for the incorporation of intravascular imaging into clinical practice.
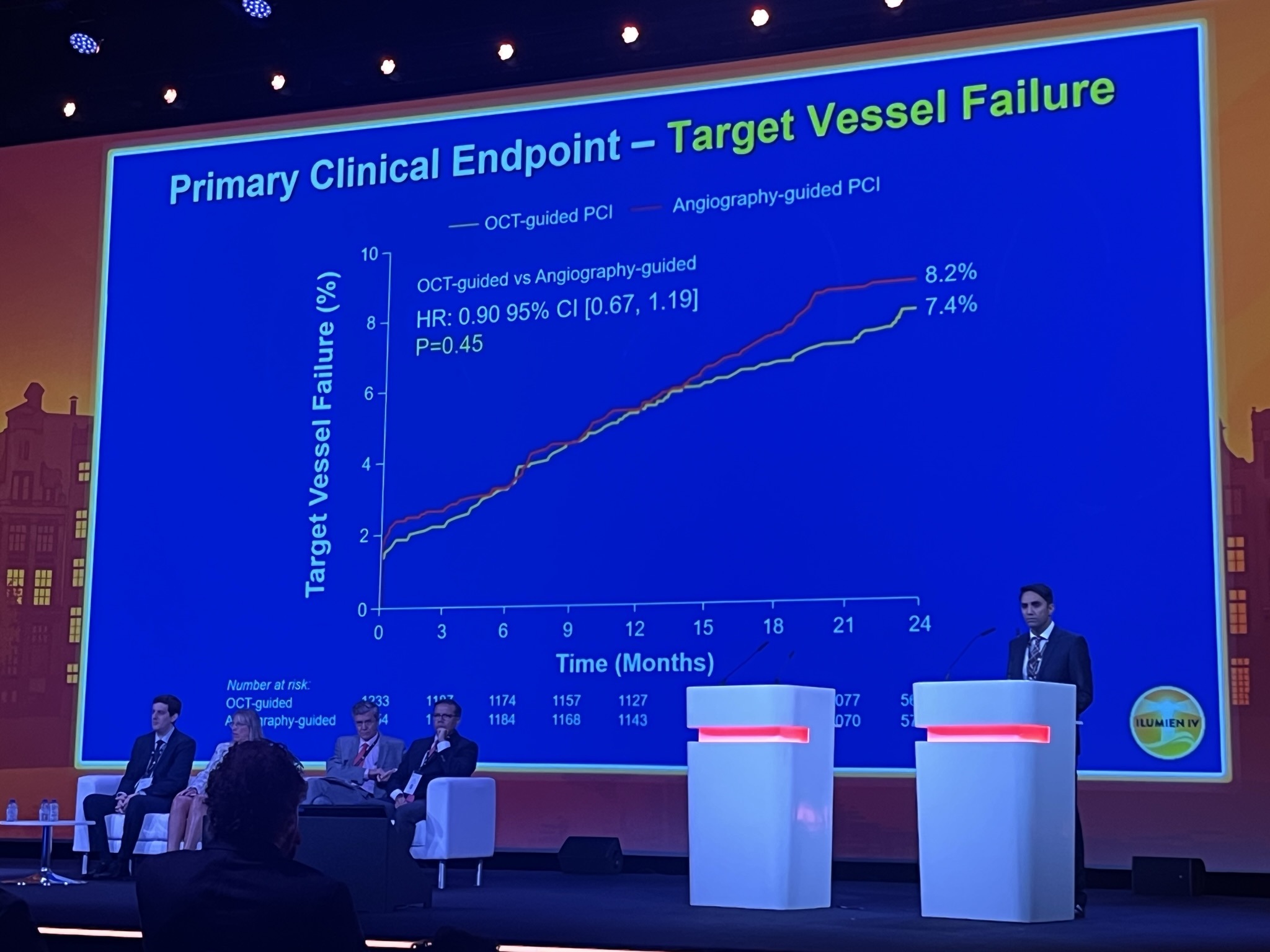
First presenting ILUMIEN IV results, investigator Ziad Ali (St Francis Hospital, Roslyn, USA) reported that the use of OCT contributed to a larger minimum stent area than when using angiographic guidance, but the trial found that there was no reduction in the co-primary endpoint of target vessel failure at two years. The impact of the pandemic on enrolment may have played a role in the neutral result, Ali said.
The trial, results of which were published simultaneously to presentation in the New England Journal of Medicine, was conducted at 80 sites in 18 countries, randomising a total of 2,487 patients to either OCT-guided PCI (1,233) or angiography-guided PCI .
Ali reported that the minimum stent area measured after PCI was 5.72±2.04mm2 in the OCT group and 5.36±1.87mm2 in the angiography group, while target-vessel failure within two years occurred in 88 patients (7.4%) in the OCT group and in 99 patients (8.2%) in the angiography group.
“OCT-guided PCI led to a larger minimum stent area, enhanced the safety of the PCI procedure and resulted in a nearly two-thirds reduction in stent thrombosis during two-year follow-up,” commented Ali of the Abbott-funded trial’s results. “However, in this trial OCT guidance did not reduce the two-year rate of target vessel failure compared with angiography-guided PCI because of a low and nearly identical rate of target vessel revascularisation in the OCT-guided and angiography-guided PCI arms.”
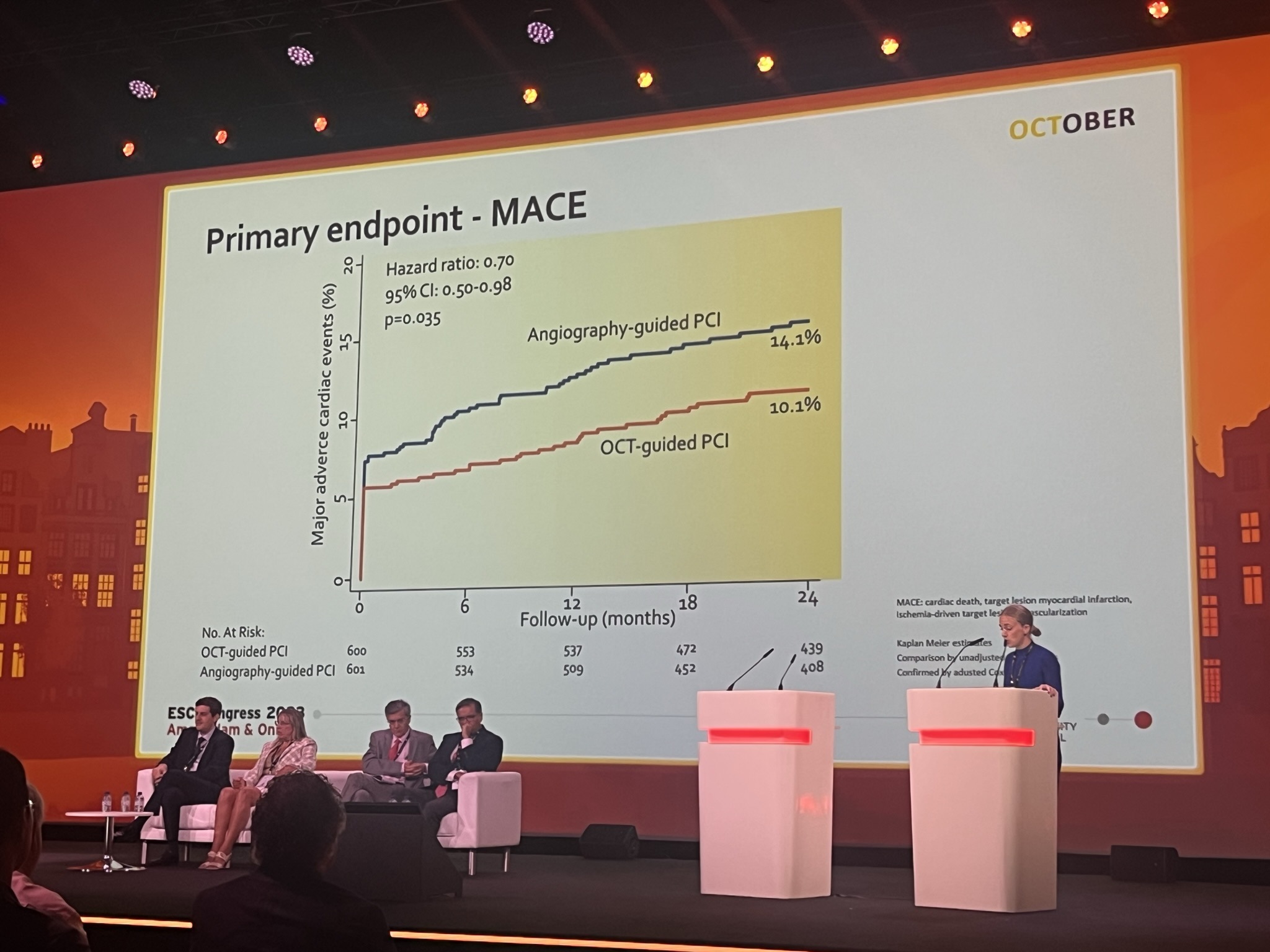
If the results of ILUMIEN IV painted a mixed picture for OCT, the following trial, OCTOBER, appeared to give a more conclusive answer into its benefit. Coming after Ali, Lene Nyhus Andreasen (Aarhus University Hospital, Aarhus, Denmark) delivered findings of the trial in which investigators examined the use of OCT in patients with complex bifurcation lesions.
OCTOBER included 1,201 patients from 38 centres in 13 European countries, and randomised 600 to OCT-guided PCI and 601 to angiography-guided PCI. Those undergoing OCT-guided PCI were treated according to a protocol including a stepwise evaluation of lesion preparation, lesion length, reference sizes, lesion coverage, stent expansion, malapposition, wire positions and ostial results. In the angiography-guided arm, the use of IVUS was allowed in cases requiring treatment of left main artery stenosis.
Reporting the results, also published in NEJM, Nyhus Andreasen detailed that the primary endpoint, major adverse cardiac events (MACE), which was defined as a composite of cardiac death, target lesion myocardial infarction, and ischaemia-driven target lesion revascularisation after two years, occurred in 10.1% of patients in the OCT-guided arm, and 14.1% of patients who underwent angiography-guided PCI.
There were no apparent differences in procedural safety, but the volume of contrast and the procedure time were both increased with OCT-guided PCI compared with angiography-guided PCI.
“The OCTOBER trial demonstrated that in patients with complex bifurcation lesions, OCT-guided PCI was associated with better outcomes after two years than angiography-guided PCI,” said Nyhus Andreasen. “Procedures using OCT guidance were safe but took longer and the investigators used more contrast. In the angiography-guided arm, IVUS was also used in approximately one in five cases, which reflects current clinical practice for complex PCI procedures in many centres. The results suggest that routine use of structured OCT guidance during PCI of complex bifurcation lesions should be considered to improve prognosis.”
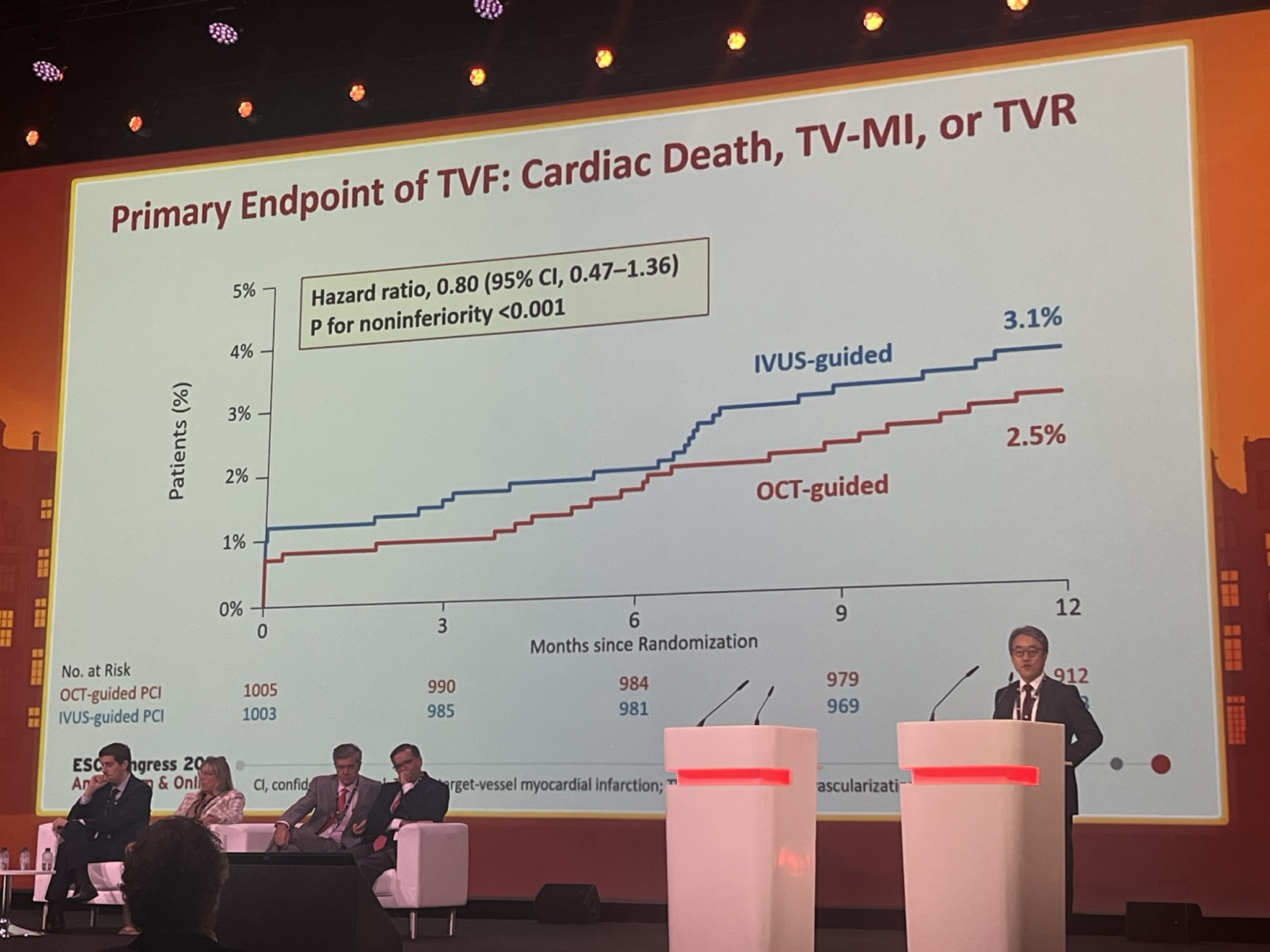
Next came the results of the OCTIVUS trial, an investigator-initiated, prospective, multicentre, randomised, open-label pragmatic trial conducted at nine sites in South Korea, in which trialists conducted a head-to-head comparison of clinical outcomes for OCT- and IVUS-guided PCI in patients with a broad range of coronary artery lesions.
A total of 2,008 patients were randomised in a 1:1 ratio to undergo either OCT-guided or IVUS-guided PCI after diagnostic coronary angiography. The primary endpoint was a composite of death from cardiac causes, target vessel myocardial infarction or ischaemia-driven target vessel revascularisation at one year, which was powered for non-inferiority of the OCT group as compared with the IVUS group.
At one year after randomisation, the primary endpoint had occurred in 25 of 1,005 patients (2.5%) in the OCT-guided PCI group and in 31 of 1,003 patients (3.1%) in the IVUS-guided PCI group. Regarding safety endpoints, investigator Duk-Woo Park (Asan Medical Center, Seoul, Republic of Korea) reported that the incidence of contrast-induced nephropathy was similar in the OCT and IVUS groups (1.4% vs. 1.5%, respectively), while the incidence of major procedural complications was lower in the OCT group compared with the IVUS group (2.2% vs. 3.7%). The total amount of contrast used was higher in the OCT group compared with the IVUS group, but the total PCI time was shorter in the OCT group.
“Among patients undergoing PCI for diverse coronary artery lesions, OCT-guided PCI was non-inferior to IVUS-guided PCI with respect to a composite of death from cardiac causes, target vessel myocardial infarction, or ischaemia-driven target vessel revascularisation at 12 months after the index procedure,” said Park. “The primary results of OCTIVUS add compelling evidence on the relative efficacy and safety of an OCT-guided strategy compared with an IVUS-guided strategy for PCI.”
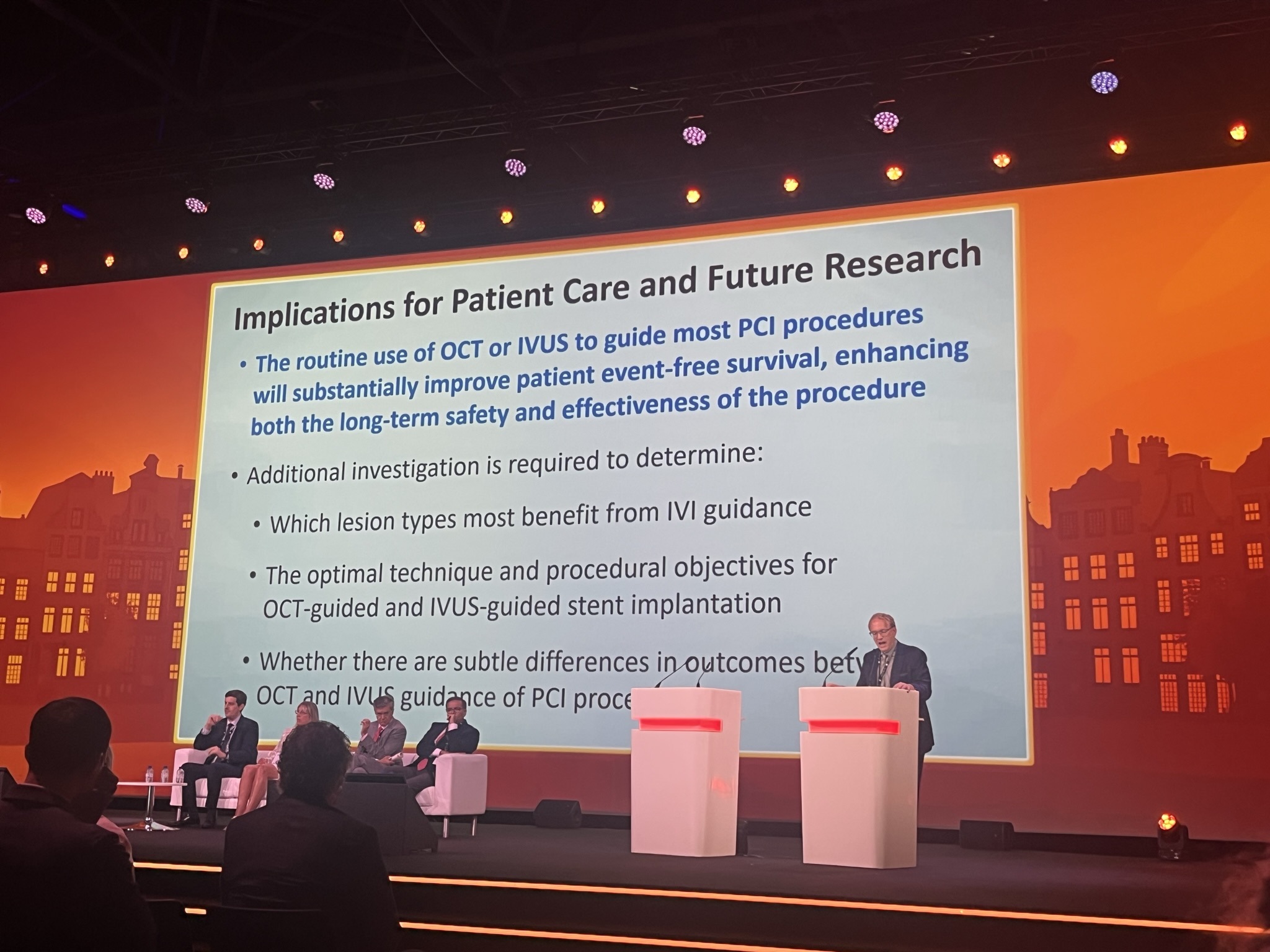
Rounding off the Hot Line session, Gregg Stone (Icahn School of Medicine at Mount Sinai, New York, USA) presented the findings of a real-time updated network meta-analysis, integrating results from both ILUMIEN IV and OCTOBER alongside prior data, to examine the effects of intravascular imaging versus angiographic guidance. The analysis compared the overall effects of imaging in improve outcomes of PCI versus angiography, as well as comparing IVUS and OCT individually to angiography and one another.
The analysis incorporated 20 randomised trials of intravascular imaging-guided PCI compared with angiography-guided PCI in 12,428 patients with chronic and acute coronary syndromes. Of those, 7,038 were randomly allocated to intravascular imaging guidance (including 3,120 patients randomised to IVUS guidance, 2,826 patients randomised to OCT guidance, and 1,092 patients randomised to IVUS or OCT guidance), and 5,390 patients were randomly allocated to angiography guidance. Patients were followed for between six months and five years.
The primary endpoint was target lesion failure, defined as a composite of cardiac death, target vessel myocardial infarction, or target lesion revascularisation. Secondary endpoints included cardiac death, target vessel myocardial infarction, target lesion revascularisation, and stent thrombosis, as well as all-cause death, all myocardial infarction and target vessel revascularisation.
Stone reported that intravascular imaging guidance of PCI resulted in reductions in the primary composite outcome of target lesion failure by 31% compared with angiography guidance of PCI. Regarding secondary outcomes, intravascular imaging guidance of PCI resulted in reductions in cardiac death by 46%, target vessel myocardial infarction by 20%, target lesion revascularisation by 29%, and stent thrombosis by 52% compared with angiography.
Alongside this, Stone also noted that there were statistically significant reductions in all-cause death, all myocardial infarction and target vessel revascularisation with intravascular imaging guidance of PCI. The outcomes were similar for OCT-guided PCI and IVUS-guided PCI when compared individually against angiography and when compared to each other.
“The results of this network meta-analysis emphasise the importance of physicians using intravascular imaging with either OCT or IVUS to optimise stent outcomes and improve the long-term prognosis of their patients,” Stone said.













