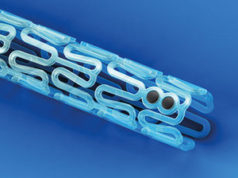
Five years after receiving the CE mark, Abbott Vascular’s bioresorbable vascular scaffold (Absorb) has been granted FDA approval—making it the first fully dissolving scaffold to be commercially available in the USA. The Absorb GT1 system, which is gradually absorbed by the body in approximately three years, is now approved for use in percutaneous coronary intervention (PCI) in patients with coronary artery disease.
The approval was based on data from the ABSORB III trial, which showed that patients who received the Absorb GT1 system had a similar rate of target lesion failure (the trial’s primary endpoint) at one year as those who received an everolimus-eluting stent with a permanent polymer (Xience, Abbott Vascular): 7.8% vs. 6.1%, respectively (p=0.007 for non-inferiority). This study also showed that there were no significant differences between devices in the rates of cardiac death, target-vessel myocardial revascularisation or device thrombosis.1
However while there was not a significant difference in the overall rate of device thrombosis between Xience and Absorb in ABSORB III, the rate of subacute device thrombosis (>24 hours to 30 days post procedure) was significantly higher with the scaffold (0.9% vs. 0.1% for Xience; p=0.04). Furthermore, two meta-analyses (published after ABSORB III) have subsequently indicated that the rate of device thrombosis is significantly higher with Absorb. For example, Kang et al—in a network meta-analysis—found that Xience, Boston Scientific’s platinum-chromium everolimus-eluting stent Promus, and Biotronik’s hybrid sirolimus-eluting stent Orsiro all have a significantly lower risk of definite/probable device thrombosis compared with Absorb.
This potentially higher risk of device thrombosis with Absorb may be mitigated by using an optimised implantation strategy. Puricel et al2 found that: “When a bioresorbable vascular scaffold-specific implantation strategy was implemented, 12-month scaffold thrombosis rates fell from 3.3% to 1.0%, an effect that remained significant when adjusted for multivariable propensity score.”
Responding to the FDA approval, Gregg W Stone (Center for Interventional Vascular Therapy, Columbia University Medical Center, New York-Presbyterian Hospital, New York, USA)—chairman of the ABSORB clinical trial programme—said: “The Absorb bioresorbable vascular scaffold represents a major advance in the treatment of coronary artery disease. This novel technology appeals to both physicians and patients alike because after treating the underlying blockage it is completely absorbed, leaving nothing behind.”

INTERVIEW: Optimal lesion preparation is the key to success with Absorb
Cardiovascular News spoke to Nick West (Papworth Hospital, Cambridge, UK), chair of the “All you need to know about BRS” session at this year’s EuroPCR (17–20 May, Paris), about how to best to implant Absorb.
What are the essential “tips and tricks” for implanting Absorb?
The key tips for success are to prepare the lesion optimally, to size and implant the device per instructions for use and to routinely optimise the result with postdilatation.
Vessel preparation should, in my view, be performed with a non-compliant balloon in all cases—with a nominal diameter sized 1:1:1 (balloon: vessel: intended scaffold diameter). Also, I think operators should have a low threshold for using cutting/scoring balloons for fibrotic or eccentrically-calcified lesions. However if you think there is a need for mechanical debulking because of extensive calcification (eg. rotablation), you should think carefully about whether or not Absorb will definitely benefit that patient.
Sizing can be undertaken either with intravascular imaging or a “poor man’s intravascular ultrasound”—imaging the non-compliant predilatation balloon at nominal diameter in two orthogonal planes to ensure full expansion and correct sizing.
Scaffold deployment should be slow, per instructions for use, to avoid damaging the polymeric structure of the device, and then routine postdilatation should be performed in every case to high pressure, ideally with a non-compliant balloon 0.25–0.5mm larger than the scaffold nominal diameter.
Of course, the importance of appropriate patient and lesion selection should not be underestimated for Absorb, and this is a part of the “learning curve” with the device. Ideally, given the slightly more involved implant procedure, operators should start with relatively straightforward lesions/cases in order to focus on the points above before transitioning to disease of increased complexity.
Gregg Stone, ABSORB II investigator, advises against using Absorb in “truly small vessels”.3 Why is this?
The data from the small-vessel post hoc analysis of ABSORB III showed an excess of clinical adverse events (both target lesion failure and scaffold thrombosis) when reference vessel diameter was <2.25mm.
This finding is not that surprising because the smallest version of Absorb available has a nominal deployed diameter of 2.5mm and devices would, therefore, have been under-expanded in the trial. Underexpansion is known to predispose to metallic stent thrombosis and this has now also been shown for Absorb, which also has a larger “footprint” (device: artery ratio). Interestingly, excess events were also seen with Xience in the small vessel analysis, confirming this is not specific to Absorb.
Aside from patients who have small vessels, are there any other patients who may not be suitable candidates for Absorb?
Any patient whose life expectancy is less than three years (the time it takes for the scaffold to resorb) will not benefit from this technology. Also while we await further data from randomised studies, use of Absorb in very complex disease states—left main stem, chronic total occlusion with dissection/re-entry, bifurcations requiring two stents—should be regarded as exploratory and not routinely recommended.
Also, if a lesion cannot be fully expanded during preparation, it will not be suitable for Absorb implantation. With the current-generation of the device, and given currently-available data, if the patient is not a drug-eluting stent candidate in the first instance particularly in terms of dual antiplatelet therapy (DAPT), they are not an Absorb candidate in contemporary practice.
If Absorb is implanted according to the “rules” (ie. not used in small vessels; routine postdilation), should we be concerned about the increased risk of device thrombosis seen with the device (in some studies)?
Although there is a consistent numerical disadvantage in terms of number of Absorb scaffold thromboses in the head-to-head comparisons, none of these differences have achieved statistical significance owing to sample size and under powering given such a low-frequency event. The trend towards excess scaffold thromboses compared with metallic everolimus-eluting stents seen in several meta-analyses is not actually that bad when the comparator for these studies—Xience—is considered. Xience has consistently been shown to have the lowest rates of stent thrombosis when compared with all other metallic stents4 and, therefore, wanting another device to be better than that Xience is a big ask. One should also consider that the studies included in these meta-analyses all reflect early experience, and techniques have already emerged that may reduce such potential risks (for example, as shown by Puricel et al).
Despite the warning signal of a potentially greater risk of device thrombosis, it is reassuring that all of the studies and the meta-analyses have shown equipoise in mortality, which may place the scaffold/stent thrombosis difference into context.
Given the ongoing debate surrounding the optimum duration of DAPT, how long would you prescribe it after implanting Absorb?
Currently, I prescribe DAPT for 12 months for all Absorb cases, similar to the current UK practice for metallic drug-eluting stents in the absence of any need for a shorter duration. There is no evidence that Absorb might require a shorter duration of DAPT than drug-eluting stents, and a study from our centre in press (Giblett et al, Eurointervention) suggests that Absorb strut coverage after acute coronary syndromes is delayed to a similar degree to metallic drug-eluting stents, meaning that we should continue to prescribe DAPT as for metallic drug-eluting stents.
Some operators have advised routine prescription of the more potent agents, such as prasugrel and ticagrelor, in preference to clopidogrel for patients receiving Absorb; this is indicated if the clinical presentation suggests this (ie. acute coronary syndromes vs. stable angina), but potent antiplatelet agents will not compensate for poor implant technique.
Therefore, at present, Absorb should not be implanted in any patients with intolerance to or non-compliance with DAPT.
Many believe that the benefits of Absorb will not be apparent until a few years after implantation. Presuming this is true, which patients may benefit the most from this technology?
This is a tough question to answer, as every interventionalist will have their own view and may answer anywhere between all patients and no patients! I think that the patients most likely to benefit will include younger patients, as they are likely to have a longer interventional “career” ahead of them in terms of need for repeat revascularisation procedures; patients with long segments of diffuse disease that would be poorly served either by metallic stenting or bypass grafting and patients presenting with acute coronary syndromes, including ST-segment elevation myocardial infarction (STEMI), where often lesions may be “softer” and disease often less extensive.
It might be better instead to reflect on where not to use Absorb—and at present, data suggest that small vessels are the principal no-go, although large vessels (outside maximal scaffold expansion diameter (3.5+0.5=4.0mm) should also be avoided in view of the potential risk of scaffold fracture. Ostial lesions have also shown a hazard for scaffold thrombosis in real-world studies, as have patients with poor left ventricular function. Very heavily-calcified lesions should be viewed with caution: as vascular function and vasomotion cannot be restored in such vessels, it is not clear whether Absorb’s putative benefits will also accrue with time in this lesion/patient group.
References
- Ellis et al. N Eng J Med 2015; 373: 1905–15.
- Puricel et al. J Am Coll Cardiol 2016; 67(8): 921–31.
- Stone. Cardiovascular News 2016; 40; 02.
- Palmerini et al. Lancet 2012; 379(9824): 1393–40.
Nick West has acted in a consultant capacity to Abbott Vascular